
Christopher Whaley PhD

https://publichealth.berkeley.edu/people/christopher-whaley/
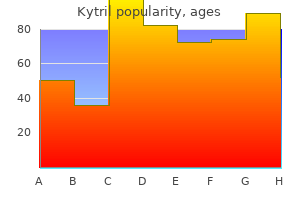
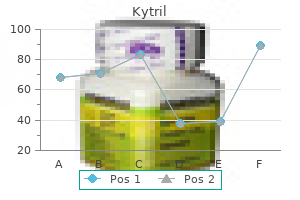
Kytril dosages: 2 mg, 1 mg
Kytril packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills

After the joint is exposed medications for schizophrenia purchase kytril 1 mg with mastercard, perform a synovectomy, carefully preserving the collateral ligaments. Tag the ends of the collateral ligaments for later repair to their tuberosity origins. Joint Preparation and Trial Implant Insertion Use a metacarpal sizing template to identify the appropriate amount of metacarpal head to be resected. Remove the metacarpal head by first making a vertical saw cut distal to the collateral ligaments. A second cut oriented 45 degrees proximally and volarly removes the remainder of the metacarpal head, retaining the collateral ligament origins. Contracture of the ulnar capsule may require detaching the ulnar collateral ligament to achieve alignment of the finger in some circumstances. Once the trial components are inserted and the joint is reduced, check component fit and position using an image intensifier. Revisions of bone cuts may be necessary for soft tissue balancing and to ensure adequate range of motion. If release of the collateral ligaments was required, drill two holes through the tuberosity at the dorsal radial and dorsal ulnar aspect of the remaining metacarpal head for reattachment of the ligaments. Closure and Soft Tissue Balancing Final Implant Insertion Irrigate the intramedullary canal with saline and 0. The joint is extended and viewed under the image intensifier before allowing the cement to harden so that lastminute corrections in alignment can be made. After the cement has cured, check passive range of motion to ensure adequate range without impingement or prosthetic binding. After hardening of the cement, tighten the collateral ligaments or reattach them to the tuberosity of the metacarpal head with nonabsorbable suture. Ensure proper radial and ulnar stability as well as rotational alignment before securing the sutures. Close any remaining capsule with absorbable suture before extensor apparatus closure. Centralize the extensor tendon and imbricate the radial sagittal bands in rheumatoid hands using nonabsorbable suture. With the finger held in slight overcorrection, imbricate the radial sagittal band over the extensor tendon. During the osteotomy, protect the origins of the radial and ulnar collateral ligaments by using small retractors or by hyperflexing the joint.
We do not routinely use intraoperative fluoroscopy; however symptoms 1974 effective kytril 1 mg, early in their experience with this procedure, surgeons may find fluoroscopy useful to confirm the position of the hardware. Symptomatic, uncontrolled shoulder instability that is recalcitrant to soft tissue or bony reconstructive procedures can be managed with fusion. Rarely, arthrodesis is indicated in young laborers with severe osteoarthritis who are poor candidates for arthroplasty because of their young age and high activity levels. Compression across the glenohumeral articular surface is achieved by placing the initial screws from the plate through the proximal humerus and into the glenoid fossa. The plate is then anchored to the spine of the scapula by a screw directed into the base of the coracoid. Contraindications the primary contraindication to glenohumeral arthrodesis is weakness or paralysis of the periscapular muscles, especially the trapezius, levator scapula, and serratus anterior. Progressive neurologic disorders that are likely to lead to paralysis of these muscles also are a contraindication. Shoulder fusion requires a significant effort by the patient to rehabilitate the shoulder and is contraindicated in patients unwilling or unable to participate in such a program. Preoperative Planning Preoperative radiographs should be evaluated for any bone defects that may require bone grafting. The skin and subcutaneous tissue are incised down to the fascia along the entire length of the incision. Anteriorly, the deltopectoral interval is developed, and the deltoid is subperiosteally elevated off the acromion, beginning at the medial aspect of the anterior head and progressing laterally and posteriorly to the posterolateral corner of the acromion. Alternatively, if the deltoid is de-innervated, as may occur following brachial plexus injury, it can be split between the anterior and lateral heads. The anterior head is then elevated medially and the lateral head laterally to provide wide exposure of the proximal humerus. Distally, the biceps tendon is identified and tenodesed to the upper border of the pectoralis major tendon. A ring or Hohmann retractor is placed on the posterior lip of the glenoid, and the humeral head is retracted posteriorly to expose the glenoid. The retractors are then removed, and the arm is extended, adducted, and externally rotated to expose the humeral head. A 1/2-inch curved osteotome or burr is used to remove the articular surface of the humerus in its entirety. The undersurface of the acromion is decorticated with a 3 /4-inch curved osteotome or burr. The arm is maintained in this position by placing folded sheets between the thorax and the extremity and having an assistant stand on the opposite side of the table to support the forearm and hand. The plate is bent 60 degrees between the third and fourth holes and then twisted 20 to 25 degrees just distal to the bend so it apposes the shaft of the humerus. With the arm supported in the appropriate position and the plate held against the scapula and humerus, a hole is drilled through the plate, through the humerus, and into the glenoid using a 3.

Alternatively symptoms 4 days before period buy kytril 2 mg on-line, the lateral decubitus position can be used with the operative limb supported by a padded bolster. Preoperative Planning Before surgery, the surgeon must ensure that the proper equipment and implants are available. A direct lateral incision with the patient supine and the arm on a hand table is used. The surgeon should use the traumatic dissection that occurred at the time of injury to gain exposure of the elbow. The underlying bones have been represented and the position of the lateral skin incision is marked with the hashed line. The arrow is pointing to the bare spot on the distal lateral humerus where the lateral collateral ligament complex has been avulsed. The ulnar nerve is at risk in this approach and should be identified and protected. The common flexor origin is split distal to the medial epicondyle to expose the coronoid medially. Alternatively, a posterior skin incision can be used with elevation of full-thickness flaps at the fascial level to approach both laterally and medially. The patient can be placed in the lateral decubitus position or supine with the arm across the chest for this approach. If the radial head is to be replaced, its excision provides excellent exposure of the coronoid through the lateral approach. If, on the other hand, it is to be fixed, set free fragments aside to allow access to the coronoid. Two parallel drill holes are made from the dorsal surface of the ulna through a separate small incision and directed toward the coronoid tip. Once the suture is passed through the capsule, its ends are brought out each of the drill holes and tied over the ulna to plicate the anterior elbow capsule. The suture ends can be retrieved through the drill holes using an eyeleted Kirschner wire, a Keith needle, or a suture retriever. Standard surgical protocol to treat elbow dislocation with radial head and coronoid fractures. Its ends will be passed through the proximal ulna and tied over the dorsal surface. This type of fixation is used if the coronoid fragment is too small to accept a screw. Once one or two guidewires are in place, they are replaced with appropriate-length screws, cannulated or regular. It is critical to tap the fragment before screw placement to avoid splitting the fragment on screw insertion.

As a result symptoms women heart attack kytril 2 mg buy on line, increases in intra-abdominal pressures are transmitted equally to the bladder and urethra and continence is maintained. Incontinence pessaries differ from pessaries for pelvic relaxation in that incontinence pessaries have added features to specifically support the urethra. Because pessaries are non-invasive, they are useful in patients for whom surgery is contraindicated (elderly, ill, or pregnant women). These devices require close medical supervision to avoid infection of the vaginal epithelium or damage to the vaginal tissues. Patients are often given vaginal estrogen to decrease the risk of vaginal trauma and ulceration. These include the abdominal retropubic urethropexies (Burch procedures), bladder neck slings, and tension-free midurethral slings (tension-free vaginal tape, transobturator tape). Most of the abdominal procedures and bladder neck slings aim to resuspend the hypermobile urethra to its normal anatomic position. Disadvantages of surgery include the risks of an invasive procedure and the risk of failure with resumption of symptoms over time. Patients with intrinsic sphincter deficiency may benefit from periurethral or transurethral placement of bulking agents to improve sphincter tone. Incontinence pessaries differ from more common prolapse pessaries in that most incontinence pessaries have a portion of the device specifically designed to support the bladder neck. The sling is supporting the urethra and bladder neck and the ends are anchored to or above the rectus fascia. Neurologic disorders such as stroke, spinal cord injury, Parkinson disease, multiple sclerosis, and diabetes mellitus can also cause detrusor overactivity (Table 19-4). Many women complain of not being able to reach the bathroom in time or of dribbling or leaking triggered by just seeing a bathroom. Detrusor overactivity presents with symptoms including urinary urgency, frequency, and nocturia. Given the wide differential for detrusor overactivity, patients should also be asked about neurologic symptoms, history of previous anti-incontinence surgery, and hematuria (suggestive of cancer, stones, or infection). Urodynamic studies should be reserved for cases resistant to initial treatment, complex cases, or if surgery is planned. Surgical treatments for urgency incontinence include sacral and peripheral neuromodulation, bladder injections, and augmentation cystoplasty. Posterior tibial nerve stimulation has been approved for urinary frequency, urinary urgency, and urgency incontinence. Rarely, augmentation cystoplasty is required in patients with severe refractory urgency incontinence. In cases where an underlying etiology is identified, it should be treated appropriately.
Due to histocompatibility mismatch treatment 02 binh discount kytril 2 mg line, these eventually separate from the wound, except in the immunosuppressed patient, and so provide only temporary coverage. Split-thickness skin grafts contain epidermis, along with a varying thickness of dermis that represents less than the full thickness of the dermis. Full-thickness skin grafts incorporate the full thickness of dermis and epidermis. Donor site refers to an area from which either a split- or full-thickness skin graft is harvested. Depending on the thickness of the graft, donor site treatment varies, from topical dressings, which typically are used for split-thickness skin graft donor sites, to direct closure, which is the usual method for addressing full-thickness skin donor defects. Skin substitutes are semisynthetic or purely synthetic constructs designed to act as replacements for lost skin structures. Their list of qualities considered to be ideal for skin substitutes still holds true more than 20 years later: Little or no antigenicity Tissue compatibility Lack of toxicity Permeability to water vapor, as would be seen in normal skin Impenetrability to microorganisms Rapid and long-term adherence to the wound bed Capacity for ingrowth of fibrovascular tissue from the wound bed Malleability, which would allow the construct to conform to the wound bed Inherent elasticity that would not impede motion Structural stability against linear and shear forces Smooth surface to hinder bacterial proliferation Good to tensile strength that would allow it resist fragmentation Biodegradability Low cost Ease of storage An indefinite shelf life Wound Bed Before making a decision about using skin grafts or a substitute, it is important to be familiar with the characteristics of a wound bed that make it suitable for grafting. In the context of upper extremity wounds, the bed specifically should contain no areas of denuded tendon or bone, as these denuded areas will not support inosculation (ie, neovascularization of the graft). Moreover, the vacuum-assisted closure device can be used over the top of a skin graft applied to a wound and, through its negative pressure effect, limit fluid collection beneath the graft, also helping to ensure contact between graft and bed through an even distribution of pressure across the interface. The lack of secondary contraction seen in full-thickness skin grafts supports their use on surfaces that overlie or are juxtaposed to joints. This lack of secondary contraction helps minimize the risk of unwanted joint contracture as the grafts mature. Over broad flat surfaces, such as the dorsal or volar aspect of the forearm, split-thickness skin grafts perform well. Wounds that involve the glabrous surface of the hand ideally are replaced with skin that possesses the same characteristics as the adjacent skin. Harvest of glabrous skin from the sole of the foot or from the contralateral uninjured hand should be considered for such use. In some cases, the wound may be so large that it is not possible to harvest sufficient donor skin while still permitting primary closure of the donor site. When this is the case, the arch within the sole of the foot may yield a full-thickness glabrous skin graft sufficient to cover the area of the original wound; however, the donor site then may require a skin graft itself. The donor site from the arch of the foot can be grafted with nonglabrous, meshed split-thickness graft with minimal morbidity due to its minimal weight-bearing requirement. Split-thickness skin graft Traditionally preferred sites have included the anterior thighs due to the ease of harvest and postoperative care of these areas. Another site that has favorable characteristics in terms of quality of graft donor, as well as healing of donor site, includes the scalp.
Drains should not be used because of the superficial nature of the elbow and the risk of deep infection symptoms type 1 diabetes kytril 2 mg otc. However, the surgeon should pay close attention to hemostasis, and for the first 12 hours a moderately tight bandage should be used to avoid hematoma formation. With triceps reattachment, the surgeon should be cautious to avoid overzealous rehabilitation for fear of compromising triceps healing, with subsequent avulsions or extension weakness. The arm is elevated on pillows or with a Bradford sling overnight to prevent edema. Nonsteroidal anti-inflammatories are avoided because of their detrimental effects on tissue healing (bone to tendon and bone to bone). On the second day after surgery the dressing is removed and the compliant patient should commence gentle active antigravity flexion, with passive gravity-assisted extension. Graduated and targeted motion is prescribed, with greater than 90 degrees of elbow flexion attempted after 5 weeks. This allows sufficient time for the triceps to adhere and heal (incompletely) to the ulna. Always, at each patient interaction, the surgeon should reiterate the restrictions of use with an elbow arthroplasty: limited internal (varus) and external (valgus) rotatory torques, 2-pound repetitive and 10-pound single-event lifting. Ray et al14 reported 5 excellent and 2 good functional results in a group of patients with an average age of 81 years at 2 to 4 years of follow-up. Gambirasio et al5 reported excellent functional results in a cohort of 10 elderly patients with osteoporotic intra-articular fractures. All 12 acute primary elbow replacements achieved excellent (n 11) or good (n 1) results. Lee et al10 reported seven acute elbow replacements for distal humeral fractures in patients with an average age of 73 years. Total elbow arthroplasty as primary treatment for distal humeral fractures in elderly patients. A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular fractures of the distal humerus in women older than 65 years. A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 65. Total elbow replacement for complex fractures of the distal humerus: an option for the elderly patient. Untreated median-nerve entrapment in bone after fracture of the distal end of the humerus: postmortem findings after forty-seven years. The results of open reduction and internal fixation in elderly patients with severe fractures of the distal humerus: a critical analysis of the results. Distal humeral fractures treated with noncustom total elbow replacement: surgical technique. Results of total elbow arthroplasty in the treatment of distal humerus fractures in elderly Asian patients. Operative treatment of type C intercondylar fractures of the distal humerus: results after a mean followup of 2 years in a series of 18 patients.
Functional outcome after minimally displaced fractures of the proximal part of the humerus treatment xdr tb order kytril 2 mg amex. Two-part and three-part fractures of the proximal humerus treated with suture fixation. The influence of displacement on shoulder function in patients with minimally displaced fractures of the greater tuberosity. Some authors believe that greater tuberosity displacement of greater than 5 mm may lead to poor outcomes. McLauglin14 first suggested that patients in whom a greater tuberosity healed with residual displacement of more than 5 mm had longstanding pain with poor function. Platzer et al21 looked at minimally displaced fractures of the greater tuberosity and found no statistical significance with varying degrees of displacement less than 5 mm. Open reduction with suture or wire fixation can achieve acceptable fixation, especially in older patients with osteoporotic bone. One study showed nearly 80% excellent results with average motion of 155 degrees of average forward flexion, 46 degrees average external rotation, and internal rotation to T11. Recent studies show promise with the use of such locking plates, although this technique is not without complications. The reproducibility of classification of fractures of the proximal end of the humerus. Conservative treatment of fractures and fracture-dislocations of the upper end of the humerus. Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Numerous techniques of internal fixation for proximal humerus fractures have been described and reported, including cloverleaf and blade plating,1 Rush pinning,15,19 spiral pinning,18 Kirschner wire and tension band fixation,3 suture and external fixation,7 and intramedullary nail fixation. Various reports have been made on the use of intramedullary nails in the proximal humerus. The method for treatment of proximal humeral fractures described in this chapter involves a minimally invasive anterior acromial surgical approach, an indirect method of reduction, and a unique intramedullary rod designed to permit a variety of proximal interlocking configurations.
On physical examination medications given to newborns buy cheap kytril 1 mg on-line, patients typically have normal external female genitalia and a short vagina that appears to end in a blind pouch. The transverse vaginal septa are usually less than 1 cm thick and may have a central perforation. It occurs when the lower vagina fails to develop and is replaced by fibrous tissue. Developmentally, vaginal atresia results when the urogenital sinus fails to contribute the lower portion of the vagina. Physical examination reveals the absence of an introitus and the presence of a vaginal dimple. Surgical correction can be achieved by incising the fibrous tissue and dissecting it until the normal upper vagina is identified. Any accumulated blood or materials can be evacuated and the normal upper vaginal mucosa is then brought down to the introitus and sutured to the hymenal ring. Once the mold is removed, dilators must still be used for several months to maintain vaginal patency. While normal sexual intercourse is possible after these surgical and nonsurgical procedures, the patient will be unable to carry a pregnancy. The nonneoplastic epithelial disorders of the vulva, including lichen sclerosis, lichen planus, lichen simplex chronicus, and vulvar psoriasis, were formerly known as the vulvar dystrophies. These lesions often require histologic examination (Table 13-2) to identify and treat the disorder and to differentiate the lesion from vulvar and vaginal intraepithelial neoplasia and cancer (Chapter 27). Lichen sclerosis is an inflammatory dermatosis that can be found on the vulva of women of all age groups, but has major significance in postmenopausal women, where it is associated with a 3% to 4% risk of vulvar skin cancer. The etiology is unknown, but several mechanisms have been proposed including immunologic, genetic, hormonal, and infectious mechanisms. The resulting atrophy can cause resorption of the labia minora, labial fusion, occlusion of the clitoris, contracture of the vaginal introitus, thinning of the vulvar skin, and skin fragility. Lichen planus is an uncommon inflammatory skin condition that can affect the nails, scalp and skin mucosa. Vulvar lichen planus is characterzed by papular or erosive lesions of the vulva that may also involve the vagina. This inflammatory dermatosis results in chronic eruption of shiny purple papules with white striae on the vulva. Similar lesions are often found on the flexor surfaces, and mucous membrane of the oral cavity. Lichen planus can be associated with vaginal adhesions and with erosive vaginitis. It generally occurs in women in their 50s or 60s and it is associated with a 3% to 4% risk of vulvar skin cancer. These patients typically have normal external genitalia, normal secondary sexual characteristics (breast development, axillary, and pubic hair), and normal ovarian function.
Mufassa, 21 years: It is important to have a good understanding of the anatomy and the most likely origin of the cyst to best plan the incision and dissection to avoid injury to important neurovascular structures. The sternal head, which lies deep to the clavicular head, is identified and isolated bluntly. It inserts on the ulnar side of the base of the middle phalanx but may attach on the radial side or have an additional insertion in the base of the distal phalanx, causing a distal interphalangeal joint contracture.
Abe, 22 years: Nonoperative management is also the treatment of choice in fractures with less than 2 mm of displacement, with minor head involvement, and without bony blockage to range of motion. After either open or arthroscopic radial styloidectomy, the postoperative dressing and sutures are removed in 7 to 10 days. The medial and lateral collateral ligaments are reattached to the epicondyles using a locking stitch that is passed through the cannulated humeral screw.
Sigmor, 37 years: Repair the lateral collateral ligament through drill holes at the center of rotation laterally. Relationship of hallux abductus angle and first metatarsal angle to severity of pronation. Primary herpes infection classically appears as multiple vesicles that develop into painful ulcers.
Flint, 43 years: In this case, a thorough examination of the vagina should be performed, and if no source is found, a subsequent examination Vignette 1 Question 1 Answer A: More than 75% of new mothers experience some degree of emotional disturbance after delivering their babies. The radial nerve passes through the supinator to gain access to the extensor surface of the forearm. Impingement after triscaphe (scaphoid-trapezoid-trapezium) fusion Rogers and Watson12 reviewed 93 patients after triscaphe fusion and found a 33% incidence of painful impingement between the fusion mass and the radial styloid that resolved after limited radial styloidectomy.
References