
Molly A. Schnirring-Judge, DPM, FACFAS
Lovegra dosages: 100 mg
Lovegra packs: 8 pills, 12 pills, 20 pills, 32 pills, 60 pills, 92 pills, 120 pills

Cystic lesions of the pancreas: an appraisal of an aggressive resectional policy adopted at a single institution during 15 years breast cancer myths buy discount lovegra 100mg line. Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors. The analysis failed to account for an increase in high-risk pathology, such as neuroendocrine tumors, and an increase in performance at low-volume hospitals. The true challenge to the dissemination of this technology is not the feasibility of the procedures, but the training of surgeons to incorporate the technology safely. At high-volume specialized centers, these procedures are safe, feasible, and efficacious; however, the dissemination process is still in an early adopter phase. The robotic interface offers many technical advantages that overcome the limitations of laparoscopic techniques while maintaining the tenets of an open approach to permit meticulous dissection and reconstruction. However, when adopting any new technology, robotic surgery imposes a significant cost and learning curve. As the field of robotics matures, further comparative studies on cost effectiveness and efficacy for improving patientcentered outcomes, such as symptomatic relief and quality of life, are needed. Laparoscopic versus open cystgastrostomy for pancreatic pseudocysts: a case-matched comparative study. Cyst gastrostomy and necrosectomy for the management of sterile walled-off pancreatic necrosis: a comparison of minimally invasive surgical and endoscopic outcomes at a high-volume pancreatic center. Safety and efficacy of videoassisted retroperitoneal debridement for infected pancreatic collections: a multicenter, prospective, single-arm phase 2 study. Videoassisted laparoscopic debridement for retroperitoneal pancreatic collections: a reliable step-up approach. Robotic total pancreatectomy with or without autologous islet cell transplantation: replication of an open technique through a minimal access approach. Fully robotic-assisted technique for total pancreatectomy with an autologous islet transplant in chronic pancreatitis patients: results of a first series. Defining criteria for selective operative management of pancreatic cystic lesions: does size really matter Mucinous cystic neoplasm of the pancreas is not an aggressive entity: lessons from 163 resected patients. Mucinous cystic neoplasms of the pancreas: imaging features and diagnostic difficulties. Pretreatment assessment of resectable and borderline resectable pancreatic cancer: expert consensus statement. Results of radical distal pancreatectomy with en bloc resection of the celiac artery for locally advanced cancer of the pancreatic body.
Syndromes
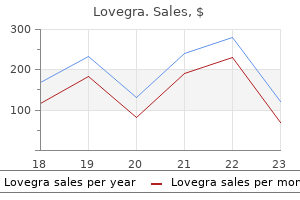
A unifying concept: pancreatic ductal anatomy both predicts and determines the major complications resulting from pancreatitis menopause insomnia discount lovegra 100mg mastercard. Selected management of pancreatic pseudocysts: operative versus expectant management. Pancreatic pseudocysts following acute pancreatitis: risk factors influencing therapeutic outcomes. Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Endoscopic transmural drainage of peripancreatic fluid collections: outcomes and predictors of treatment success in 211 consecutive patients. Percutaneous drainage of pancreatic pseudocysts is associated with a higher failure rate than surgical treatment in unselected patients. Surgical management of complications associated with percutaneous and/or endoscopic management of pseudocyst of the pancreas. The effect of size of giant pancreatic pseudocysts on the outcome of internal drainage procedures. Duct drainage alone is sufficient in the operative management of pancreatic pseudocyst in patients with chronic pancreatitis. Pancreatic pseudocysts complicated by splenic parenchymal involvement: results of operative and percutaneous management. Laparoscopic and endoscopic approaches for drainage of pancreatic pseudocysts: a systematic review of published series. Incidence and management of pancreatic and enteric fistulas after surgical management of severe necrotizing pancreatitis. The significance of sinistral portal hypertension complicating chronic pancreatitis. Extrahepatic portal hypertension in chronic pancreatitis: an old problem revisited. Improved outcomes in postoperative and pancreatitis-related visceral pseudoaneurysms. Treatment of chronic pancreatitis complicated by obstruction of the common bile duct or duodenum. Systematic review and meta-analysis of somatostatin analogues for the treatment of pancreatic fistula.
A single-institution experience with fistulojejunostomy for external pancreatic fistulas young women's health tips 100mg lovegra order free shipping. Endoscopic and Minimally Invasive Therapy for Complications of Pancreatitis Christopher G. When complications such as inflammatory pancreatic fluid collections develop, however, interventional therapies are often required. The new definitions and classifications of inflammatory pancreatic fluid collections as distinct entities are important to recognize as the natural history, risk of subsequent morbidity and mortality, and outcomes of minimally invasive therapies are varied. Furthermore, the majority of antecedent literature reporting the outcomes of management is based upon heterogeneous combinations of these inflammatory fluid collections. In concert with the medical technology expansion, the revised Atlanta definitions for inflammatory pancreatic fluid collections have provided more homogeneous data on outcomes and clinical management strategies. Given the heterogeneity of pancreatic fluid collections, local technical expertise, and anatomic variation, management decisions should be individualized within the context of a multidisciplinary team composed of surgeons, radiologists, and gastroenterologists. Approximately 15% to 20% of patients develop pancreatic and peripancreatic necrosis,1 but in these cases, ductal disruption is invariable and complications are more frequent and illness is protracted. These collections often do not require any therapeutic intervention as they are generally sterile, lack a well-defined, mature wall, and self-resolve after a few weeks. However, if they become infected or symptomatic, therapy may need to be considered. As a part of the spectrum of disease, these inflammatory conditions can result in local complications that necessitate invasive treatment. In the past decade, less-invasive endoscopic, percutaneous, and laparoscopic therapies to address these complications have been developed in an effort to reduce the morbidity associated with traditional open surgical techniques. Rapid expansion of medical technology continues to evolve clinical management strategies, and revised definitions for inflammatory pancreatic fluid collections have provided more homogeneous data on outcomes. Given the heterogeneity of clinical manifestations, local technical expertise, and anatomic variation, the therapies chosen should be individualized, preferably within the context of a multidisciplinary team of surgeons, gastroenterologists, and radiologists, taking into account the natural history and pathophysiology of the disease process. The significant mortality (11% to 39%) and complication rates (34% to 95%) associated with open necrostectomy,16,17 including the development of pancreaticocutaneous and enterocutaneous fistulas, incisional hernias, and exocrine and endocrine pancreatic insufficiency, led to the development and implementation of less invasive techniques, such as endoscopic necrosectomy and percutaneous drainage. As a result, clinical guidelines, including the International Association of Pancreatology and the American Pancreatic Association evidence-based guidelines, endorse percutaneous catheter or endoscopic transmural drainage as the first step in the treatment, followed by either endoscopic or minimally invasive surgical necrosectomy. Once access is secured, the tract is dilated using a graduated dilating catheter, needle knife sphincterotome, or cystotome, and subsequent dilation to 15 to 20 mm is performed using a balloon dilator to allow passage of an upper endoscope into the necroma. Preservation of the tract is achieved by the placement of stents into the cavity across the gastric or duodenal wall.
In those patients undergoing laparoscopic hepatic resection for cancer menstruation icd 9 100 mg lovegra for sale, there was no difference in 3- or 5-year overall survival when compared with well-matched open hepatic resection cases. Estimated intraoperative blood loss, Pringle time, total and pulmonary complication rates, and hospital length of stay were significantly lower for the laparoscopic group. Median operating room time was 234 minutes (range, 60 to 555 minutes) and blood loss was 200 mL (range, 20 to 2500 mL), with 10% receiving a blood transfusion. Median length of postoperative hospital stay for the entire series was 4 days (range, 1 to 22 days). The median interval from primary colon surgery to liver metastasectomy was 12 months (range, 0 to 60 months). At 1, 3, and 5 years, overall survival rates were 88%, 69%, and 50%, respectively, whereas disease-free survival rates were 65%, 43%, and 43%, respectively. At a median follow-up of 30 months, the 5-year overall survival for the laparoscopic group was 64%, versus 56% for the open group (P =. The recurrencefree survival at 5 years was 30% for the laparoscopic and 20% for the open group (P =. The laparoscopic group had a shorter time to ambulation, initiation of oral intake, and length of hospital stay. With a median follow-up of 30 months, there were no differences in overall survival. There were no significant differences in rates of blood transfusion, operative time, or positive margins between the groups. During the Second International Consensus Conference on Laparoscopic Liver Resection held in Morioka, jury recommendations and expert technical recommendations were discussed and summarized. As mentioned previously, major robotic hepatectomy has only limited data available for evaluation at this current time. Laparoscopic donor liver surgery should be performed under institutional ethical approval and reporting registry. Surgeons must also begin with minor laparoscopic resections before embarking on the more complex ones. Conceptual changes include the caudal approach that optimizes hilar dissection and transection of the liver parenchyma for major and/or anterior resections. The lateral approach (left lateral decubitus position) can be used to optimize access to lesions located in posterior segments. Although individual hilar dissection is considered the standard technique by many surgeons, the Glissonian approach is feasible and can be useful for anatomic liver resection, especially hemihepatectomy, sectionectomy, or less. Although it can reduce operative time, this approach needs expertise, skills, and thorough knowledge of liver anatomy. Energy devices are efficient and reliable, but they should not replace the acquisition of basic skills of hepatic surgery, such as meticulous dissection, direct visualization, and proper sealing of the vascular structures.
For sphincterotomy menopause neuropathy lovegra 100mg for sale, the ampulla is then incised sufficiently along the anterosuperior side (opposite the pancreatic duct orifice) to permit removal of the impacted calculus. The sphincter is usually divided sequentially between small clamps, with sequential suture approximation of the duodenal and bile duct mucosa. A 2- to 3-cm longitudinal choledochotomy is made close to the lateral border of the duodenum along with a similar-sized longitudinal duodenotomy at the corresponding location. All participants attained the mastery standard after a short period of targeted practice. Spontaneous passage of bile duct stones: frequency of occurrence and relation to clinical presentation. Ultrasonic evaluation of common bile duct stones: prospective comparison with endoscopic retrograde cholangiopancreatography. Useful predictors of bile duct stones in patients undergoing laparoscopic cholecystectomy. Selective use of preoperative endoscopic retrograde cholangiopancreatography in the era of laparoscopic cholecystectomy. Selection criteria for preoperative endoscopic retrograde cholangiopancreatography before laparoscopic cholecystectomy and endoscopic treatment of bile duct stones: results of a retrospective, single-center study between 1996-2002. Magnetic resonance imaging of the common bile duct to exclude choledocholithiasis. Endoscopic sphincterotomy for prevention of the recurrence of acute biliary pancreatitis in patients with gallbladder in situ. Endoscopic management of common bile duct stones leaving the gallbladder in situ: a cohort study with long-term follow-up. Early laparoscopic cholecystectomy improves outcomes after endoscopic sphincterotomy for choledochocystolithiasis. The algorithm proposed is only a guideline, and ultimate treatment will depend on physician experience and available resources. Hospital cost categories of one-stage versus twostage management of common bile duct stones. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Prospective evaluation of a selective approach to cholangiography for suspected common bile duct stones. A prospective single-blinded controlled study comparing laparoscopic ultrasound of the common bile duct with operative cholangiogram. Laparoscopic intracorporeal ultrasound versus intraoperative cholangiography: after the learning curve. Meta-analysis of the diagnostic accuracy of laparoscopic ultrasonography and intraoperative cholangiography in detection of common bile duct stones.
Fish Liver Oil (Cod Liver Oil). Lovegra.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96995
Blunt abdominal trauma resulting in gallbladder injury: a review with emphasis on pediatrics menstruation every two weeks causes order lovegra 100 mg without prescription. The goal of percutaneous biopsy is to obtain a core of tissue with good preservation of the underlying hepatic architecture. The presence of significant ascites or underlying coagulopathy is a relative contraindication to percutaneous biopsy. However, transjugular biopsies are best used for large and easily targetable lesions and are of limited use for small focal lesions because of the inability to accurately place the needle. Furthermore, the amount of tissue obtained is often smaller and more fragmented compared with percutaneous core needle biopsies, making pathologic assessment more difficult. If multiple percutaneous attempts have failed to obtain adequate material, if there is suspicion that a liver lesion is highly vascularized and prone to bleeding, if there is a need to obtain tissue from multiple sites, or if it is otherwise preferable to biopsy the liver under direct vision, then either laparoscopic or open liver biopsy may be used. Preoperative laparoscopy, as a diagnostic tool in hepatobiliary malignancies, has been discussed extensively during the past two decades. Although no definitive consensus has been achieved, with the improvement of modern radiographic imaging modalities its role appears to be limited to select cases. A particular case is represented by gallbladder and hilar cholangiocarcinoma where the yield of staging laparoscopy and ultrasonography is relatively high and the value of surgical palliation is relatively low, thus arguing in favor of laparoscopic staging in order to prevent an unnecessary laparotomy. The incision should be placed over the inferior edge of the liver but should be at least 3 cm below the costal margin to allow for adequate fascial closure. The liver can be examined both visually and by palpation, but care should be taken to not disturb any portosystemic collateral vessels. If these friable vessels are disrupted, or if the hepatic capsule is ruptured during examination, a major abdominal operation may be required to gain control. Visual inspection for gross evidence of cirrhosis, nodularity, abnormal color or texture, or neoplasm may be revealing. A laparoscopic ultrasound probe can be used through a small incision, or, if the incision is large enough, the regular probe may be used. A core needle biopsy can be obtained through the same site, directed deeper into the liver parenchyma but away from the porta hepatis. If significant bleeding is expected, hemostatic 2-0 chromic catgut or Vicryl mattress sutures can be placed in an interlock V shape outside the biopsy site prior to biopsy. After the biopsies are taken, the base of the biopsy site is treated with the argon beam coagulator for hemostasis. The fascia should be closed with running permanent suture if ascites is anticipated. Similarly, the skin should be closed with a running long-lasting suture if ascites is anticipated. Superficial lesions can be biopsied under direct visualization using cupped biopsy forceps, whereas deeper lesions might require laparoscopic ultrasound guidance and the use of percutaneous core needle biopsy devices. In addition, the direct laparoscopic visualization of the liver parenchyma allows for quick identification and treatment of any potential bleeding complications caused by a large needle biopsy.
Water will follow the flow of electrolytes to maintain an isotonic environment between the tissue and intestinal lumen breast cancer jerseys lovegra 100mg buy online. In the proximal small intestine, water freely flows into the cell through permeable tight junctions between enterocytes. The tight junctions become less permeable in the distal intestine, where water requires active transport to enter the cell. Sodium, chloride, bicarbonate, calcium, and iron are all absorbed in the small intestine. Potassium, magnesium, phosphate, and other ions are also absorbed through the intestinal mucosa. Solutes such as glucose, amino acids, short-chain peptides, and bile acids are absorbed via cotransport with Na+. The absorption of Na+ leaves the luminal contents electronegative and the cell and paracellular space electropositive. The fat-soluble vitamins A, D, E, and K are transported and absorbed similarly to dietary fats. They are taken up by micelles and transported into the enterocyte, where they are packaged into chylomicrons and then taken up into the lymphatic system. The water-soluble vitamins are absorbed in the jejunum and ileum by active or passive transport (Table 71. First, intrinsic factor, secreted from gastric parietal cells, couples with vitamin B12. The complex then binds to a membrane receptor at the terminal ileum and is absorbed. Once in the cell, the complex dissociates and vitamin B12 enters the portal circulation. There is much that is known about the mechanisms by which these disease states occur, but further understanding of the molecular and genetic organization of the small intestine will serve to enhance clinical care. Extrinsic nervous control of motility of small and large intestines and related sphincters. Development of the enteric nervous system and its role in intestinal motility during fetal and early postnatal stages. Stimulation of betaadrenoceptors with isoprenaline inhibits small intestinal activity fronts and induces a postprandial-like motility pattern in humans. Positive correlation between symptoms and circulating motilin, pancreatic polypeptide and gastrin concentrations in functional bowel disorders. Parathyroid hormone activates vitamin D by stimulating the conversion of 25-hydroxycholecalciferol to 1,25-dihydroxycholecalciferol, which is the active form of vitamin D.
A combination of aldosterone antagonist and loop diuretic is optimal menstrual reg lovegra 100 mg on line, but there is no consensus as to the exact ratio of one to the other. As indicated earlier in this chapter, one of the early vascular responses to portal hypertension is marked arterial vasodilation of the splanchnic circulation. This in turn leads to a hyperdynamic systemic circulation, decreased systemic vascular resistance, and lowered blood pressure. This in turn activates the vasoconstrictor and antinatriuretic systems that affect the kidneys, with sodium and water retention and renal vasoconstriction. The inability of the kidneys to excrete sodium is thus the first event, with water retention subsequently leading to dilutional hyponatremia. This gives the deceptive laboratory picture of low serum sodium yet high total body sodium. A second pathologic factor in the development of ascites is the hepatic sinusoidal change. Cirrhosis results in high intrasinusoidal pressure and further damage to the already discontinuous endothelium of the sinusoid. This high pressure leads to excess fluid filtration through the sinusoid, and much of the ascitic fluid forms from the liver surface. Removal of 4 to 6 L of ascetic fluid during paracentesis is occasionally necessary. Circulatory dysfunction due to volume shifts can be minimized by concomitant infusion of albumin if necessary. The major limitation of large-volume paracentesis as a treatment for refractory ascites is the frequency at which ascites will reaccumulate. As frequently as once a month may be required in some patients, although more frequent paracentesis warrants further intervention. A clinical diagnosis of ascites should be made on physical exam, often appearing with unexpected weight gain, peripheral edema, and abdominal distention demonstrable by fluid wave on exam. A diagnostic paracentesis should be performed on all patients with cirrhosis when they first present with ascites. The fluid (30 to 50 mL) should be sent for cytologic examination, albumin concentration, total protein content, white blood cell counts, and differential and bacterial culture. Refractory ascites portends a poor prognosis and the need for more aggressive therapy. Specific pulmonary vascular disorders related to chronic liver disease and portal hypertension are increasingly well understood. Contrast echocardiography, lung perfusion scanning, and pulmonary angiography have classically been used to diagnose pulmonary vasodilation. A hundred percent oxygen inspiration can measure the degree of oxygen shunting if Pao2 fails to rise above 300 mm Hg; however, this is not present in all patients. Patients with Pao2 of less than 50 mm Hg who are going into liver transplant have poorer survival rates than those with Pao2 greater than 50 mm Hg.
If esophagogastric variceal bleeding from leftsided portal hypertension occurs menopause questions for doctor 100 mg lovegra buy with visa, splenectomy is the definitive treatment. Splenic artery embolization is another option for symptomatic patients medically unfit for surgery. Some authors have argued that splenic vein thrombosis patients with asymptomatic gastric varices undergoing pancreatic surgery for another indication (chronic pain, pseudocyst, etc. Rarely in the setting of acute necrotizing pancreatitis there will be direct erosion by a pseudocyst or necrotic collection into a major vessel such as the portal vein or splenic artery. More commonly, pseudoaneurysms will form adjacent to a pseudocyst or an area of pancreatic necrosis due to enzymatic breakdown of a small arterial wall from contact with pancreatic secretions. Late hemorrhagic complications including pseudoaneurysm, diffuse bleeding from pancreatic necrosis, and pseudocyst bleeding appear to complicate 1% to 4% of pancreatitis cases. In a series by Balthazar and Fisher, these complications typically presented late, anywhere from 2 months to 8 years (mean 2. Coil embolization is the usual technique, but stent placement can be used if the target artery cannot be sacrificed, such as with a common hepatic or proper hepatic artery pseudoaneurysm. Pseudoaneurysm communication with the gastrointestinal tract or exposure to pancreatic juice over time may lead to infection and rebleeding. Emergent surgery has an important role for control of bleeding when a patient is hemodynamically unstable or when attempted angiographic embolization of the bleeding vessel is unsuccessful. Proximal and distal ligation of the bleeding vessel is usually the most expedient procedure, although limited pancreatic resection may also be performed. Obstruction due to pseudocyst compression can occur anywhere along the gastrointestinal tract from the stomach to the colon. After pseudocyst decompression, obstruction should resolve unless the pathophysiology of pancreatitis has caused adjacent ischemia and fibrosis. In rare cases, infarction of the mesentery or bowel wall has caused intestinal necrosis or perforation requiring emergent resection and proximal stoma. It is important to have a multidisciplinary approach to treatment including surgeons, endoscopists, radiologists, and interventional radiologists. Understanding the status of the main pancreatic duct is essential for selecting the optimal therapies. There are many scenarios in which surgery remains the most efficient and effective treatment strategy. Incidence, risk factors and clinical course of pancreatic fluid collections in acute pancreatitis. Incidental pancreatic cysts: clinicopathologic characteristics and comparison with symptomatic patients. Association between advances in high-resolution cross-section imaging technologies and increase in prevalence of pancreatic cysts from 2005 to 2014.

Normal peak systolic velocity in the celiac artery is less than 160 cm/second pregnancy 8th month cheap lovegra 100 mg with visa, with end-diastolic velocities of less than 55 cm/second. An abnormal fasting peak systolic velocity of greater than 200 cm/second is predictive of a greater than 70% to 99% diameter reduction. Abnormal fasting peak systolic velocities of greater than 275 cm/second are predictive of a greater than 70% to 99% diameter reduction. Much research has been done to define luminal stimuli that are responsible for postprandial hyperemia. Some mechanical stimulation of mucosa elicits a hyperemia response, but chyme does not produce enough mechanical stimulation necessary to increase intestinal blood flow. Osmolality of a meal can dilate vasculature if luminal osmolalities exceed 1500 mOsm/kg, but there is no response at lower osmolalities. Bile causes glucose and long-chain fatty acids to become vasoactive29,30 but does not increase jejunal blood flow. Ileum B Arteries of jejunum and ileum Characteristic Color Caliber Wall Vascularity Vasa recta Arcades Fat in mesentery Circular folds (L. Intestinal absorption of nutrients is required to initiate a vasomotor response that leads to an intestinal hyperemia. Extrinsic neurohumoral mechanisms also contribute to the control of intestinal blood flow. Splanchnic organs receive 25% of cardiac output and contain 25% of total blood volume at rest. Neural regulatory control of the mesenteric circulation is mostly sympathetic and is mediated by alpha receptors. This response causes constriction of the mesenteric arterioles and capacitance vessels. Preganglionic cholinergic fibers of the greater splanchnic nerves synapse at the celiac ganglia. Postganglionic adrenergic fibers of the celiac ganglia cause mesenteric artery and arteriolar vasoconstriction. During a fightor-flight response, vasoconstriction occurs in the mesenteric vascular bed. This shifts blood flow from the temporarily less important intestinal circulation to the more crucial areas of the heart and brain. Parasympathetic fibers of the vagi innervate the intestine but exert little effect on the mesenteric vasculature. Capillary filtration and microvascular permeability increase in the small intestine. Ischemic injury to the intestine occurs when blood flow is reduced to levels at which oxygenation and nutrients to the tissue are compromised. Acute mesenteric ischemic syndrome etiologies in the adult include occlusive disease (embolic or thrombotic), nonocclusive disease, and mesenteric venous thrombosis. The best clinical indicator of the presence of acute intestinal ischemia is severe abdominal pain that is out of proportion to physical findings.
Jared, 43 years: The appearance of solid nodules, irregularity or thickening of the cyst wall, a tumor size larger than 6 cm, and the presence of metastatic lesions and/or peripheral eggshell calcifications are additional criteria that are concerning for malignancy. Although some asymptomatic patients spontaneously develop arterial collaterals and can be treated conservatively, most survivors with late hepatic artery thrombosis will ultimately require retransplantation. It is not usually appropriate in a septic, hypotensive patient and does not enable a satisfactory examination of the retroperitoneal duodenum.
Fadi, 30 years: Careful attention must be paid to the physiologic, metabolic, and immunologic derangements in these patients. Care should be taken to note a replaced or accessory left hepatic artery running in this location. This facilitates inspection of the posterior aspect of the head of the gland, as well as the posterior wall of the duodenum, and provides a view of the suprarenal inferior vena cava.
Pavel, 24 years: One final, but extremely important, potential contraindication to transplantation is any prior history of extrahepatic malignancy in the candidate. The risk of pancreatitis is reduced by placement of the catheter as distal as possible to avoid particulate agent going to nontarget sites. Transit disorders of the gastric remnant and Roux limb after Roux-en-Y gastrojejunostomy: relation to symptomatology and vagotomy.
Miguel, 45 years: The impact of preoperative immunosuppressive drugs on surgical outcomes is controversial. These fibers consist of both cholinergic and noradrenergic neurons; however, the sympathetic innervation of the stomach and duodenum is largely inhibitory. Experience with resection of the pancreas in the treatment of chronic relapsing pancreatitis.
References