
Najamul H. Ansari, MD
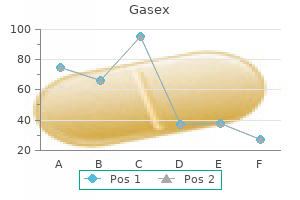
Gasex dosages: 100 caps
Gasex packs: 1 bottle, 2 bottle, 3 bottle, 4 bottle, 5 bottle, 6 bottle, 7 bottle, 8 bottle, 9 bottle, 10 bottle

Eilber Karyn Schlunt gastritis fiber purchase gasex 100 caps, Nirit Rosenblum, Raz Shlomo, et al: Surgical therapy for uterine prolapse. Florian-Rodriguez Maria E, Hare Adam, Chin Kathryn, et al: Inferior gluteal and other nerves associated with sacrospinous ligament: a cadaver study, Am J Obstet Gynecol 215(5):646. Good Meadow M, Abele Travis A, Balgobin Sunil, et al: Vascular and ureteral anatomy relative to the midsacral promontory, Am J Obstet Gynecol 208(6):486. Kenton Kimberly, Pham Thythy, Mueller Elizabeth, et al: Patient preparedness: an important predictor of surgical outcome, Am J Obstet Gynecol 197(6):654.
Lily (Lily-Of-The-Valley). Gasex.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96312
Randomized Trials of Adjuvant Chemotherapy There have been multiple randomized trials set forth to define the role of adjuvant chemotherapy (Table 137 gastritis natural cures generic 100 caps gasex otc. Unfortunately, these trials have not provided sufficient evidence to support adjuvant chemotherapy, and this is because of low numbers, difficulty with patient accrual, early termination of the trials, and flawed statistical design. Three-year time to progression was significantly better in the chemotherapy group, with 70% of patients free from disease compared with 46% assigned to observation. Although this trial did demonstrate an advantage in favor of adjuvant chemotherapy, it has been criticized for several reasons. This trial also highlighted the difficulty of administering chemotherapy after cystectomy with 25% of patients who were assigned to receive chemotherapy and who were not receiving therapy. Three-year disease-free survival was significantly improved in the chemotherapy arm (63% vs. This study was updated with a total of 83 patients (38 received chemotherapy after the close of the trial based on the interim analysis). Ten-year follow-up data maintained an advantage in the chemotherapy group with regard to progression-free survival (44% vs. Ultimately, 92% of patients in the observation arm showed evidence of tumor progression compared with 27% who received chemotherapy. Overall, the number of patients is small because of early closure of the trial after interim analysis. Many patients in the observation group were not offered chemotherapy at the time of disease progression and, as one would expect, not all patients randomized to chemotherapy ultimately received such therapy. Since the mid-2000s, there have been several attempts at large-scale adjuvant chemotherapy trials, most of which have been presented in abstract form. The chemotherapy cohort was randomly assigned to one of two regimens; either gemcitabine 1000 mg/m2 days 1, 8, and 15 and cisplatin 70 mg/m2 day 2 or the same gemcitabine schedule plus cisplatin 70 mg/m2 day 15, every 28 days. There was also no statistical difference in disease-free survival in the observation (42. The initial study was designed to randomize 610 patients in a 1: 1 fashion but was closed early because of poor accrual. The smaller sample size resulted in significant underpowering of the study in detecting a significant difference between adjuvant chemotherapy and observation. The accrual goal in this trial was 800 patients; however, the study was terminated for poor accrual, and ultimately fewer than 100 patients enrolled.
Serum studies have shown total anticholinergic burden can be measured helicobacter pylori gastritis diet discount gasex 100 caps with mastercard, although lists of medications must be used in conjunction with this to improve diagnostic accuracy (Lampela et al. Increased anticholinergic burden can worsen underlying cognitive function, memory, and associated comorbid conditions such as Alzheimer disease (Fox et al. Increased anticholinergic load has been associated with increased risk of mortality and decline in physical function (Fox et al. Attempts should be made to reduce or eliminate use of anticholinergics to the extent possible. Reductions in overall anticholinergic burden have been associated with improvements in behavioral and cognitive outcomes in affected elderly patients (Kersten et al. In cases in which these medications are used for a evidence-based document that categorizes medications into different groups based on characteristics and considerations for use in older adults. The most recent version includes information regarding level of evidence used to make recommendations, and overall strength of the recommendation from the expert panel. This document is being maintained and updated on a regular basis as new data emerge. This can help them to make more informed decisions about medication use in older adults, which can help improve the care they provide (Griebling et al. Identification of alternate medications or treatment strategies may be helpful in this regard (Hanlon et al. Some medications are considered always inappropriate for elderly patients and should be avoided in all cases. An example of such a medication often used in urologic practice is meperidine (Demerol). This drug was included because of the significant potential risks for delirium and other adverse events caused by accumulation of a toxic metabolite, poor overall efficacy, and availability of other more clinically useful alternatives. In this case, these medications should be avoided or used with caution in older adults with a history of chronic constipation or cognitive impairment. A basic principle for prescribing medications in the geriatric patient population is to "start low and go slow. Starting with lower doses and gradually increasing medication dosing with time can help to alleviate some of these potential problems. One caveat that must be considered is that medication dose may have to be increased to reach the point of clinically efficacy. Therefore care should be taken to avoid keeping doses of medications so low that they are not actually effective for symptoms they are prescribed to treat. Dose escalation should be continued until a clinically effective end point, maximum dosing for a particular medication, or intolerable side effects are reached. Because of side effects from this medication, they develop new symptoms that are attributed to a different cause, leading to prescription of a second medication to treat the side effects. To avoid this problem, clinicians should consider whether a new symptom may be due to a medication side effect rather than another cause.
Patients with urethrovaginal fistulae resulting from synthetic slings should be counselled that de novo or persisting stress incontinence can occur and that additional conservative or surgical treatment may be necessary (Blaivas and Mekel gastritis symptoms tagalog gasex 100 caps buy amex, 2014; Lee and Zimmern, 2016; Reisenauer, 2015). This patient reported ongoing urinary incontinence for 10 years after an endoscopic bladder neck suspension. Labial and Vaginal Flaps and Neourethra the simplest flap is a vaginal advancement flap (Fall, 1995). This labial skin can be used as a patch to cover the urethral defect but can also be used to create a tubular neo-urethra (Jiang et al. The numbers of patients reported are small, and there are no data on the long-term outcome of fistula closure and continence rates. The underlying bulbocavernosus tissue can be incorporated in the pedicled flap and probably offers a better vascularization and more bulking to the repair. This could allow a safer placement of a sling afterward, in those cases in which bothersome stress incontinence would occur postoperatively (Candiani et al. Only 1 out of the 8 had a fistula recurrence, while 3 out of 4 of the conventional repairs broke down; however, these cases were not randomized between surgical techniques (Rangnekar et al. The indications for Martius flap in the repair of all types of fistula remain unclear. In some cases the fistula repair can be combined with a Martius flap and an autologous sling with good results (Chodisetti et al. Transvaginal urethrovaginal fistula closure was performed followed by a pedicled rectus abdominis muscle flap interposed between the fistula closure and vaginal suture line. The muscle flap was based on the inferior epigastric vessels and provided additional support to the urethra, bladder neck, and bladder base. Urethrovaginal fistula repair with the rectus abdominis muscle flap was successful in all cases without recurrence. Of the patients 5 (83%) were continent and able to void to completion at a mean follow-up of 23 months (range 2 to 66). Once the diagnosis is made on cystoscopy, the bladder is examined for additional fistulae. Video-urodynamics may accurately characterize any associated incontinence, including that associated with detrusor dysfunction, although this will not often influence the decision to close the fistula. Treatment of Urethrovaginal Fistulae Several techniques for urethrovaginal fistula closure have been described. Surgical correction intends to create a continent urethra that permits volitional, painless, and unobstructed passage of urine. Depending on the size, localization, and cause of the fistula and the amount of tissue loss, urethral reconstruction techniques may be necessary to restore the urethra and to achieve postoperative continence (Blaivas and Purohit, 2008). Vaginal Approach Goodwin and Scardino (1980) described in their series that a vaginal approach yielded a success rate of 70% at first attempt and 92% at second attempt, but that an abdominal approach only leads to a successful closure in 58% of cases.
Although most patients are hesitant about this potential requirement gastritis chronic erosive buy 100 caps gasex mastercard, it is rare for a patient to decide against an orthotopic diversion because of this once he or she has been educated about it. Urethral Stricture Disease or External Sphincter Damage Severe urethral stricture disease in men and women is a contraindication for orthotopic diversion. Poor external sphincter function in a man who is highly motivated to undergo orthotopic diversion may be managed with a concomitant or delayed artificial urinary sphincter device (Simma-Chiang et al. Similarly, a woman with significant stress incontinence might undergo a concomitant Burch or pubourethral sling procedure, although she is likely to be dependent on intermittent catheterization to drain properly if this is done. Prior Pelvic Radiation It is not uncommon for patients to require surgical management of invasive bladder cancer after previous failed radiation therapy or after radiation treatment of a prior pelvic malignancy. Patients with prior radiation are at increased risk for several complications, even with an ileal conduit diversion. Kim and Steinberg (2001) found an increased risk for surgical complications, especially those that required percutaneous or surgical intervention, in 23 patients undergoing cystectomy and conduit after radiation compared with 23 matched controls. They found that ureteroileal complications occurred in 9% of patients by 5 years and concluded that it was not necessary to use transverse colon for diversion in these patients. The complications and ultimate functional outcome of orthotopic neobladders in patients with prior pelvic radiation have been evaluated by a number of authors. Patients who have had a prior radical prostatectomy may have a particularly difficult dissection around the proximal urethra at the prior vesicourethral anastomosis. The location and health of the proximal urethra can be assessed endoscopically both preoperatively and at surgery, and acceptable continence can be obtained in selected patients assuming that they had good continence before cystectomy (Huang et al. Nine patients had fair or poor continence before surgery, and 6 of those underwent artificial sphincter placement either at the time of cystectomy or afterward. However, 11 of the 13 men with good preoperative continence, including 1 who had both radical prostatectomy and radiation, regained good continence (0 or 1 pad Chapter 141 per day) after neobladder construction. One challenge in these surgeries is to identify the prior vesicourethral anastomosis to ensure that the bladder is entirely resected. Flexible cystoscopy at the time of the apical dissection can assist in this regard. In conclusion, with careful dissection a patient who was continent after the initial radical prostatectomy surgery can be expected to have an acceptable result with a neobladder. A patient with multiple prior bowel resections may be at risk for developing chronic diarrhea or even short bowel syndrome after an additional 45 to 60 cm of small bowel is resected. In these patients, alternatives to orthotopic diversion such as a sigmoid neobladder might be entertained. In general, prior bowel resections can be managed by carefully dissecting out all of the small bowel, taking down any adhesions before performing the diversion. It is critical to identify the old bowel anastomosis and, whenever possible, take it down and use that site as one end of the continent reservoir. This avoids potential devascularization of the bowel segment between the old and new bowel anastomoses. Orthotopic Urinary Diversion 3239 direct contact with the fibers of the levator ani muscle.
A guidewire is placed through the stricture gastritis medication list generic gasex 100 caps visa, and progressive dilation is performed until it is 18-Fr (if possible). Two-Stage Urethroplasty this is a standard technique to treat longer strictures at the phallic urethra. The urethra is opened, and marsupialization is obtained by suturing the borders of the urethra to the borders of the skin incision. In case of a narrow and/or severely scarred urethral plate, the plate can be resected and replaced or augmented by a full-thickness skin graft or by oral mucosa. At least 3 months later, if the urethral plate has healed well, the borders of the marsupialized urethra are incised and retubularized around a urethral catheter. Endoscopic Incision (Direct Vision Internal Urethrotomy) Endoscopic incision is done under sedation (if the phallus is not sensitive yet) or under spinal/general anesthesia. This period is required as it is skin that needs healing and not urethral mucosa, surrounded by spongiosal tissue. Flap Urethroplasty Substitution urethroplasty with local phallic or scrotal skin flaps is of limited use seen the paucity of mobile local tissues and the risk for penile/scrotal deformities after local flap harvest. For complex or recurrent stricture at the phallic urethra, a complete urethral substitution at this part needs to be performed. Options are a radial forearm free flap or a superficial circumflex iliac artery free or pedicled groin flap. They can present themselves to each urologist with urologic problems, which is why insight into the reconstructive techniques and possible complications is useful for every urologist. The aim of this chapter was to provide any urologist with essential knowledge to be able to take care of acute urologic problems. Thereafter, referral to experienced centers for treatment of the complications is advisable. Definitive Perineostomy the technique is the same as for contemporary perineostomy in the early postoperative phase. The perineum is incised at the midline until the fixed part of the urethra is reached. Urethral Hair Growth In case the urethra is made from skin flaps (which is usually the case), hair growth can occur in the urethra. If a skin flap will be used for the phallic urethra, a flap from a region with no or minimal hair growth is harvested. Related symptoms are difficulty voiding, local irritation, and urethral discharge. Once it has formed, the phallic urethra is opened at the ventral side with removal of the stone (if present). The borders of the urethra are sutured to the borders of opened skin of the phallus. In the next stage, the urethral plate is tubularized as during the second stage of a two-stage urethroplasty.
Syndromes
Penalver Manuel gastritis diet xp gasex 100 caps buy on line, Mekki Yasir, Lafferty Heather, et al: Should sacrospinous ligament fixation for the management of pelvic support defects be part of a residency program procedure
The curve toward the native urethra is abrupt gastritis que es gasex 100 caps order online, and two small sinuses toward the orifices of Bartholin glands are present bilaterally from this native urethral meatus in which the tip of the catheter can get stuck. One attempt of blind catheterization with a Tiemann tip catheter can be performed, but this attempt must be aborted in case of any problems. A second attempt can be performed with the use of a Freudenberg mandarin by which the sharp curve at the native female urethral meatus can be passed easily. However, in case of any difficulties, it is better to stop and do a flexible cystoscopy with placement of a guidewire into the bladder to avoid provoking urethral trauma (and subsequent stricture formation). In the early postoperative period, the fistula is evident if the urethral catheter is visible through the wound dehiscence. As there is usually an association with delayed healing of the phallus, further maceration of the wound should be avoided. For this purpose, the urinary diversion (transurethral or suprapubic catheter) is maintained until this issue is resolved. After this period, the urinary diversion can be removed, and the patient can start to void through the fistula. Smaller fistulas have a high chance (up to 70%) of spontaneous closure (Monstrey et al. If the fistula persists for longer than 3 months, it is assumed to be permanent, and a surgical closure will be required. The fistulous tract is excised with closure of the urethra and skin and with interpositioning of a healthy layer between both. As no dartos layer is available in these patients, only local fatty tissue can be used for coverage. Compared with the male urethra, which consists of mucosa in spongiosal tissue, the phallic urethra is based on skin from the flap in which healing is delayed. Again, stricture formation is usually related to healing problems of the phallus and most commonly occurs at areas with a poorer blood supply. This is the reason why the majority of strictures are located at the phallic part of the urethra, the anastomosis, or the external meatus (Lumen et al. This is a mucocutaneous junction that is prone to stricture formation enforced by delayed healing as a result of poorer blood supply at the extremities of the flap. Most of the strictures at the anastomotic site are short and will usually appear short after phallic reconstruction. As in males, transmen with urethral stricture will present with a typical plateau curve on uroflowmetry. Urethral Complications in Transmen Up to 40% of patients will suffer urethral complications after phalloplasty. Urethral Fistula A urethral fistula is a very common early postoperative complication (35%) (Monstrey et al. The most common location is at the base of the phallus followed by fistulae at the shaft of the phallus. Perineal fistulae are rare because of the better coverage of the urethra with Chapter 134 Special Urologic Considerations in Transgender Individuals 3071 Endoscopic incision has a success rate of 44%.
Dmochowski R gastritis diet to heal gasex 100 caps buy without a prescription, Blaivas J, Gormley E, et al: Female stress urinary incontinence update panel of the American Urological Association Education and Research, Inc.
From Finland the rate of vesicovaginal fistula was reported to be 1 in 1250 after all hysterectomies gastritis urination discount 100 caps gasex fast delivery, 1 in 455 after laparoscopic, 1 in 1000 after total abdominal, and 1 in 5000 after vaginal hysterectomy (Harkki-Siren et al. The publicly available tables from the national hospital database in England give similar figures of 1 in 600 after total abdominal hysterectomy, and 1 in 5000 after vaginal hysterectomy (Herbert et al. More detailed longitudinal analysis of patientlevel information from the same data set suggests a rate of 1 in 788 for all types of hysterectomy, 1 in 540 for abdominal hysterectomy for benign disease, 1 in 896 after vaginal hysterectomy for benign disease (excluding prolapse), and 1 in 3861 after vaginal hysterectomy for prolapse (Hilton and Cromwell, 2012). Ketamine abuse can lead to not only severe changes in the bladder wall structure but also fistula formation, as was shown in 14. The operative approach to hysterectomy is an important factor, because bladder injuries are at least three times more common during abdominal hysterectomy compared with vaginal hysterectomy. Hilton calculated the risk for fistula formation in radical hysterectomy for cervical cancer to be 1 of 87, whereas in vaginal hysterectomy for prolapse, the risk was only 1 of 3861 (Hilton and Cromwell, 2012). It has been suggested that patients with severe abdominal pain, distention, paralytic ileus, hematuria, or symptoms of severe irritability of the bladder after abdominal hysterectomy be investigated early for a possible bladder injury (Kursh et al. Vaginoscopy has been suggested as an adjunct measure, in some cases, using a modified endoscope or flexible cystoscope to visualize precisely the fistula tract (Andreoni et al. A visual and manual assessment of inflammation surrounding the fistula is necessary, because it may affect timing of the repair. Significant inflammation, infection, or induration around the fistula may mitigate against immediate repair. Relevant vaginal anatomy, including depth, associated prolapse, atrophy, and introital size are carefully recorded, because these may affect the surgical approach to repair. Anatomically, fistulae located high in the vagina, at the level of the hysterectomy cuff in a deep narrow vagina, may be best approached by some surgeons abdominally because a vaginal approach in these patients can be challenging. Postmenopausal vaginal atrophy may be treated with preoperative topical estrogen replacement, thereby optimizing the health and vascularity of potential reconstructive flaps. Palpation for masses or other pelvic pathology, which may require attention at the time of fistula repair, is also performed. Notation of prior incisions in the perineum, lower abdomen, and thigh is necessary because these tissues may be required for flap reconstruction when definitive repair is undertaken. Small or occult fistulae may be identified in this fashion (Drutz and Mainprize, 1988; Hanash et al. The vagina may be packed with gauze (3-swab test) or directly inspected for blue-tinged leakage (Gannon, 1990). If the vaginal packing remains dye free with this maneuver, then the possibility of a ureterovaginal fistula can be investigated with the use of clean vaginal packing, intravenous indigo carmine (or other vital dye), and a repeat pad test. Blue staining at the proximal end of the pad after this maneuver suggests the presence of a ureterovaginal fistula.
Dan, 50 years: This patient with advanced multiple sclerosis underwent surgical bladder neck closure and ileovesicostomy (ileal chimney). Lightner D, Rovner E, Corcos J, et al: Randomized controlled multisite trial of injected bulking agents for women with intrinsic sphincter deficiency: mid-urethral injection of Zuidex via the Implacer versus proximal urethral injection of Contigen cystoscopically, Urology 74(4):771�775, 2009. It is important to consider if and how findings from urodynamic testing may change treatments. The third surgical principle in constructing the continence mechanism is the use of the intussuscepted nipple valve or the flap valve, which avoids the need for intussusception.
Renwik, 65 years: Jejunal Conduit the jejunum has the largest diameter of the small bowel and the longest mesentery. Kanai K, Kikuchi E, Ohigashi T, et al: Gemcitabine and paclitaxel chemotherapy for advanced urothelial carcinoma in patients who have received prior cisplatin-based chemotherapy, Int J Clin Oncol 13(6):510�514, 2008. Patients with stress urinary incontinence following urethral reconstructive surgery may be offered artificial urinary sphincter and should be counseled that complications rates are higher (Sandhu et al. In cases of severe obstruction, a nephrostomy tube may be placed to enable more accurate characterization of renal function after relief of obstruction.
Snorre, 47 years: Because of the risk of litigation, some mesh kit manufacturers have removed their products from the market. Direct inspection by urethroscopy is suggested in lieu of urethrography in female patients with suspected urethral injury (Koraitim, 1999; Perry and Husmann, 1992). In this case, these medications should be avoided or used with caution in older adults with a history of chronic constipation or cognitive impairment. Raz S: Modified bladder neck suspension for female stress incontinence, Urology 17:82�85, 1981.
Harek, 25 years: Regardless, en bloc resection provides a viable approach to intravesical management of appropriately selected tumors. A transperitoneal, extravesical approach offers a wide working space and permits creation of both refluxing and nonrefluxing anastomoses. Organizational factors can be as important as clinical medicine and nursing issues in this setting (Yoon et al. Adjuvant Chemoradiation Multiple studies have demonstrated that patients with locally advanced disease (pT3�4) have high pelvic failure rates (20% to 40% at 5 years) and that perioperative chemotherapy does not significantly improve that risk (Baumann et al.
References